UMass Memorial Health: In-Home Hospital Care Focused on Equity
“Where would you rather receive care?” This is the question the UMass Memorial Hospital at Home team has repeated over and over. They asked leadership and stakeholders this question to solidify buy-in. They posed it to physicians to build engagement and garner referrals. And for three months, they’ve offered this question to dozens of patients, nearly always hearing the same response “I’d like to go home.”
UMass Memorial Health’s Ongoing Challenges
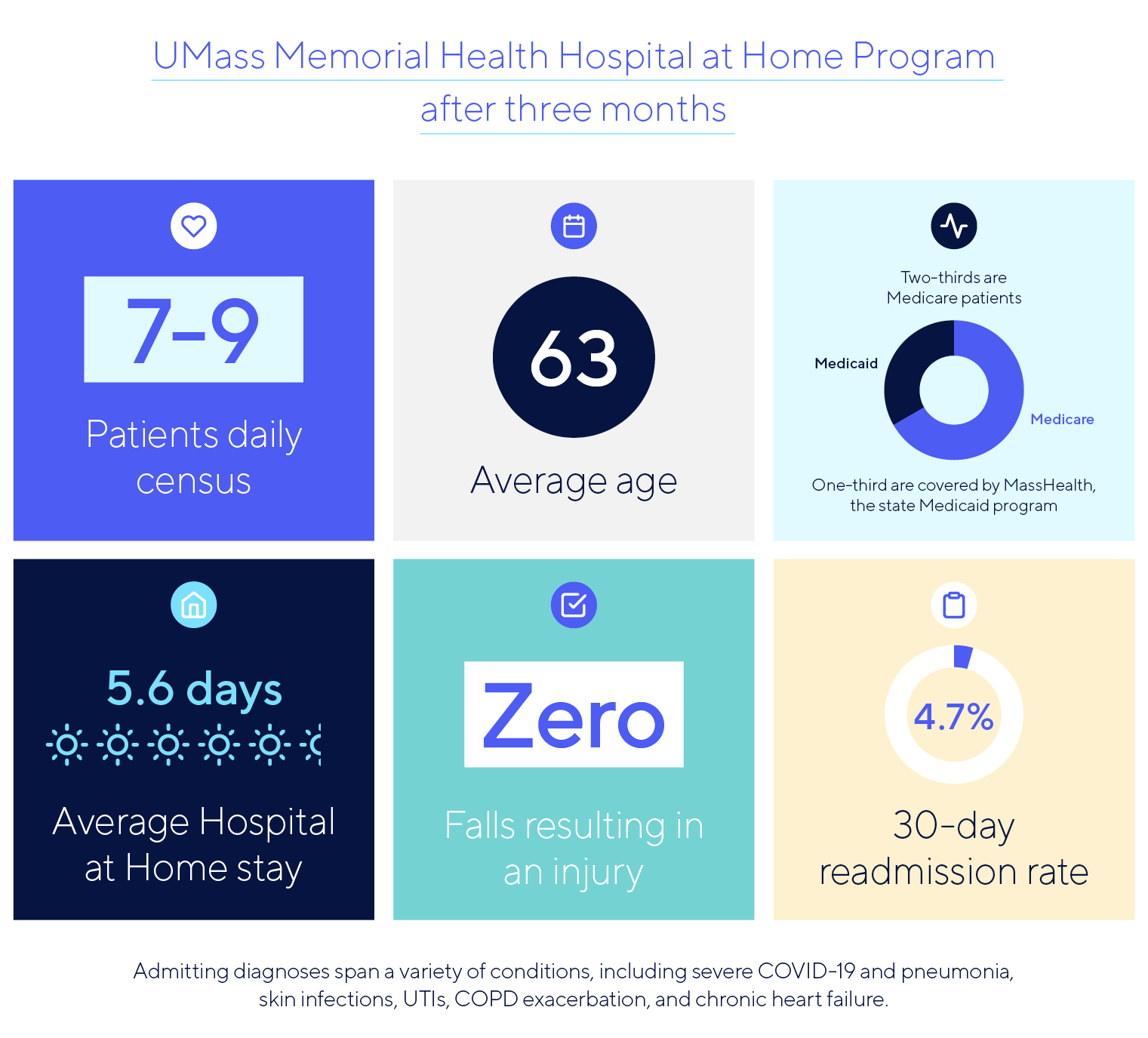
In less than six months, the team at UMass Memorial Health planned, built, and launched a Hospital at Home program from their academic medical center serving central Massachusetts. With the fewest hospital beds per capita of any health system in the state, UMass Memorial has made expanding capacity a top priority. “We provide care to more than half of the Medicaid population in the region, and we’re consistently operating at or near capacity,” says Dr. Constantinos (Taki) Michaelidis, Medical Director for the Hospital at Home program. The new Hospital at Home program is helping them scale acute care outside brick-and-mortar facilities.
“If you can bring higher acuity care into the home, patients just do better.”
Dr. Constantinos Michaelidis, Medical Director, Hospital at Home
In a recent webinar, Dr. Michaelidis was joined by Candra Szymanski, Interim AVP for Hospital at Home, to explain how they built the UMass program, the lessons they learned, and the promising results they’re already seeing.
Hospital Care at Home is a Strategic
Long-Term Initiative
In addition to better serving an under-bedded population, the UMass team also identified the need for a value-based solution and more flexible inpatient capacity as they plan for growing inpatient demand. They see the Hospital at Home model as a strategy for addressing all of these needs.
For UMass Memorial, delivering hospital care at home is not a short-term solution to pandemic-driven challenges. “Our leadership sees Hospital at Home as a strategic long-term initiative, not an experimental pilot,” says Dr. Michaelidis. He points to this emphasis as key to the alignment across stakeholders that helped them move quickly to build this service offering.
Acute Care Focused on Patient Equity
The UMass team’s focus on underserved and low-income patients drove them to place equity at the center of their program. “There’s a misconception in the industry that Hospital at Home is only for patients who live in large, comfortable houses,” says Dr. Michaelidis. “But there’s data to suggest low income patients actually benefit disproportionately from this care model.”
Interim AVP for Hospital at Home, Candra Szymanski, explains: “This care model helps us discover SDOH factors that we wouldn’t otherwise be aware of. This discovery opens the door to addressing food insecurity, medication reconciliation, care coordination with a PCP, and so many services to shore up patients’ environment and keep them safe.”
“We’re able to get the whole picture of how patients are living and the complex factors affecting their health.” –
Candra Szymanski, Interim AVP, Hospital at Home
One role that has been instrumental in pursuing patient equity: the case manager. This team member coordinates with various agencies and community resources and ensures patients get access to ongoing support services, improving health and wellbeing long after discharge.
A key tool that helps UMass extend hospital care at home into a variety of living situations: the Current Health tablet and Home Hub. By offering a pre-configured tablet with video calling and multiple language options, and a connectivity hub requiring only a standard electrical outlet, UMass can deliver safe acute care in almost any home.
Szymanski says, “When it comes to admitting patients to our Hospital at Home program, language is not a barrier to us. With our Current Health device, our patients don’t even have to have internet access to receive acute care in their home.”
Early Metrics from the UMass
Hospital at Home Program
The UMass Memorial Hospital at Home program is an inpatient med/surg floor in the home, adhering to all hospital and CMS quality and safety requirements.
Listen to the full story from UMass Memorial Health
in our on-demand webinar:
Building a Hospital at Home Program from the Ground Up