Day in the Life of a Hospital-at-Home Team
With the extension of the CMS Acute Hospital Care at Home waiver, Hospital at Home programs are poised to continue growing.
Research shows up to 25 percent of the total cost of care for Medicare fee-for-service (FFS) and Medicare Advantage beneficiaries could shift from traditional care facilities to the home by 2025—translating to roughly $265 billion worth of care services.
This trend also equates to a rapidly increasing need for skilled nurses and other providers who can deliver this quality day-to-day care. But what is that day like? Keep reading to better understand what the provider side of this experience looks like.
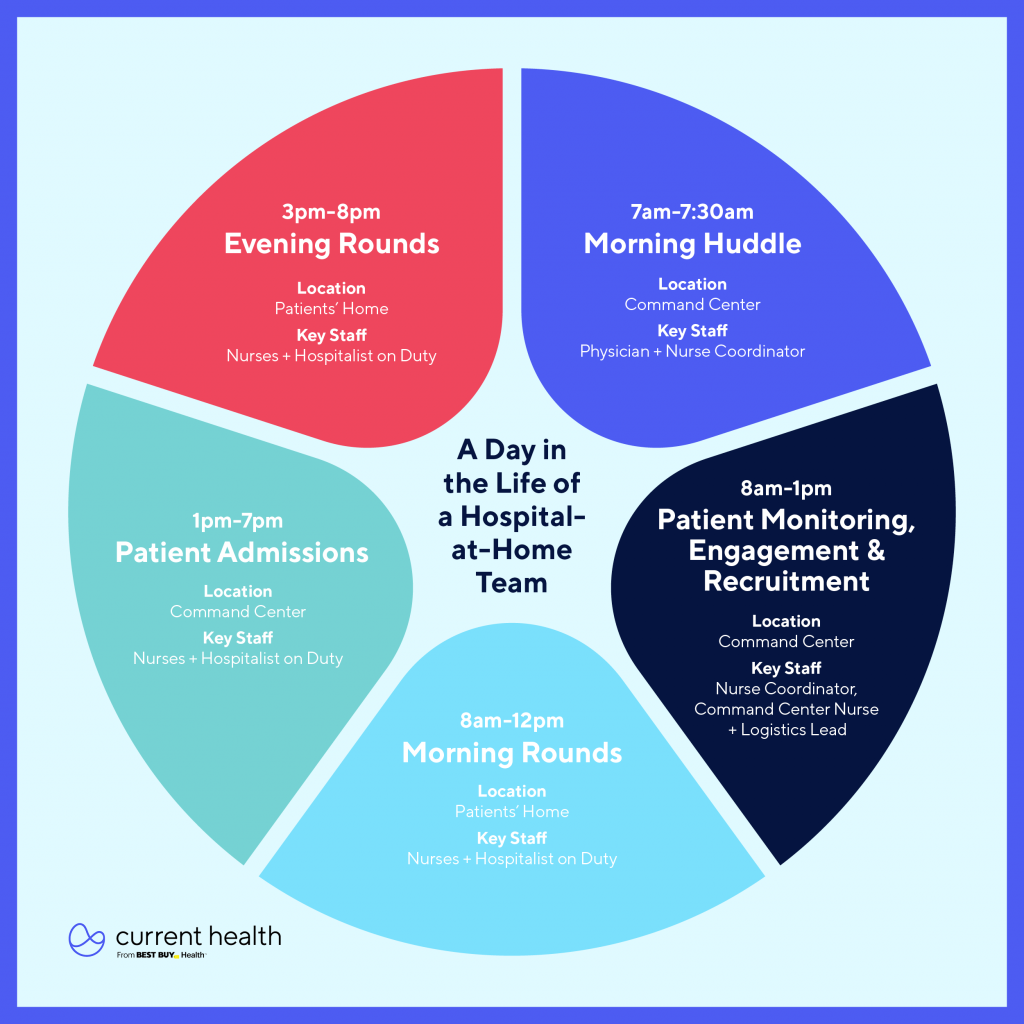
Morning Huddle: 7 am
Key Staff: Nurse Coordinator
What’s Happening: Mornings begin with a huddle at the physical Command Center. A nurse coordinator and physician review patients on the census, as well as go over the staffing model for the day and needs from other departments. One more review is then conducted—of home health candidates in the pipeline from inpatient floors.
Deployment: 7:30 am
Key Staff: Nurse Coordinator, Field Nurses
What’s Happening: Nurses deploy for morning rounds from their own homes or the hospital’s physical Command Center. A phlebotomist is deployed, if needed. Nurses take oxygen machines and other durable medical equipment (DME) as needed from the Command Center or other DME providers are called and scheduled to deploy equipment at a patient’s home. Homes can be anywhere from 5 to 40 minutes away from the Command Center.
When patient Gary and his wife arrive at home, they’re joined by a care team member who helps set up their equipment and monitoring devices. This will allow the Command Center team to observe his condition remotely.
Morning Rounds: 8 am to 12 pm
Key Staff: Nurses, Hospitalist on Duty
What’s Happening: Nurses arrive at patient homes for their morning rounds. Each nurse completes 2-3 visits, depending on the census. Visits begin with greetings, then core vitals are taken, and any medications and IVs needed are administered. The nurse asks the patient about the previous night, answers questions and considers goals of care. Any needs or changes to DME is discussed. Blood is taken, if required. The nurse records notes throughout the visit in the electronic medical record (EMR) on a laptop or through an app. Before the nurse leaves, everyone participates in a video visit with the hospitalist on duty.
Gary’s care team provides the services that the physician ordered. Toward the end of the visit, they video conference with the hospitalist on duty, who talks with Gary and his wife about his treatment and expectations over the coming days.
Reporting: 8 am to 1 pm
Key Staff: Nurses, Hospitalist on Duty
What’s Happening: A nurse is deployed for admission and arrives at Gary’s home, as close to his arrival as possible. After greeting the patient and any family members, the nurse discusses what will happen next.
The nurse proceeds by conducting medication reconciliation, setting up any oxygen, activating the Current Health kit, and taking core vitals. Other topics the nurse discusses with the patient and family include how to use the kit and what it does; how monitoring works; and how to get in touch with a nurse. The nurse initiates a brief video call between the home hospitalist, the patient, and family member to ensure all questions are answered.
If not already complete, the nurse or Clinical Coordinator initiates DME orders and meal service, and schedules in-home labs. All relevant data flows back and forth between the EHR and the Current Health platform.
Evening Rounds: 3 pm to 8 pm
Key Staff: Nurses, Hospitalist on Duty
What’s Happening: Nurses deploy for evening rounds from their homes or the physical Command Center and a phelmbotomost is deployed, if needed. A nurse or nurse coordinator who has the home visit schedule will call patients who are expecting a visit at night (based on the previous day’s plan).
Gary receives his prescribed treatment and his care team monitors his progress. After the in-person provider leaves, virtual providers are standing by, watching vital signs and symptoms. These virtual providers are positioned to deploy in-person medical assistance if they foresee a problem, worrisome trend or if something unexpected.
Watch our on-demand webinar for advice on staffing your care-at-home program.


![[Webinar Recording]This Way Home: Top 10 Predictions for Care at Home in 2025](https://www.currenthealth.com/wp-content/uploads/2025/01/DSG-846-JAN-WEBINAR-LINKEDIN-16_9-AD2-P2.jpg)