Ten Tips for a Successful Care-at-Home Program
Care at home is on the rise. From chronic care management to Hospital at Home and virtual ward, healthcare providers are rethinking the types of care that can safely be delivered while the patient stays at home. But operationalizing these new programs presents a series of challenges that your team will need to address to reach cruising altitude.
Through a series of interviews with patients and clinical staff, we found the following ten program elements contribute directly to the success of care at home. These elements fit into one of three general categories: process, team, or technology.
Efficient and Sustainable Processes
- Create a simple referral process to drive adoption.
Referrals are key to getting your program off the ground, retaining staff, and growing patient capacity. Ideally, you want multiple referral sources and a simple process to get patients into your program. Consider each referral source in terms of the process and engagement:
- How much work does it take to refer a patient to the program? When and where does that work occur?
- How are we helping referral teams remember our care at home program as an option when evaluating patients?
The Rapid Response team at Croydon NHS identified the option to make referrals 24/7 as helping to drive adoption of their virtual ward program. This was especially helpful in securing referrals from emergency departments and ambulance services.
Learn more about engaging referring providers.
- Dedicate resources for logistics to maximize patient reach.
For higher acuity programs, logistics management is critically important. Your program must plan for transporting remote monitoring kits and DME, as well as equipping field nurses with all the supplies they need for in-home visits. Depending on your program’s size and staff, it may be appropriate to outsource some logistics services to a partner like Current Health, but your team will still need to plan for staff logistics if in-home visits are within the scope of your program.
- Ensure patients know what to expect.
When informing and consenting a patient for care at home, the process begins at the initial site of care. This is where patient education and suitability for care at home should begin. Then, care at home teams should contact patients directly to assess the safety of their home and potentially help set up in-home technology. When possible, the consenting process should also include the patient’s family member. Understanding the monitoring process helps both patients and family members feel at ease.
Here’s what one patient’s family caregiver had to say about their experience:
“The doctors and nurses made me aware [patient] was not in a good way and they thoroughly explained about them being linked to the monitor….it was amazing, I would have been really scared without it and it really helped a few times when they [patient] got really bad. They [nurse] told me everything I needed to know and anything else they were just on the other end of the laptop… and not just a voice, you can see and speak to them on video.”
This perception of security and support is what care at home teams should aim for as they educate and admit patients for care at home.
- Build protocols for emergency treatment.
Every care-at-home program should have care escalation protocols that are appropriate to the patient cohort. Responding to emergent care needs will look different based upon the structure of your organization and local emergency services. Responding to serious alarms for patient vital signs should begin with contacting the patient or their in-home family member. After understanding the situation, the care at home team may help coordinate emergency response to help ensure care continuation.
Note: some clients who operate lower-acuity programs opt not to monitor patients overnight, instead instructing patients to contact local emergency services during that time.
- Prioritize patient discharge and care coordination.
The question of “what happens next for this patient?” is incredibly important for the patient experience, staff alignment, and clinical outcomes. Within higher acuity programs, discharged patients may need continuing in-home care from a community-based or home care service. For Hospital at Home programs, plan for field nurses to spend about an hour providing patient education, answering questions, and collecting monitoring devices.
Plan for what handoffs look like from a technology and patient data perspective. How are orders for follow up care placed, and how does the team ensure the next step in the patient’s care journey has taken place?
“My COPD has improved since the respiratory team took over and helped me with rehabilitation. I still do the exercises when I need them. They helped me get back to where I should be before the infection.”
Patient describing their improved outcomes
- Plan for patient follow-up communication after discharge.
Post-discharge communication ensures patients receive the follow-up care, equipment, and support they need to avoid readmission and safely stay at home.
Depending on the type of care at home program you have, this communication and coordination may be primarily focused on care continuation through home care or primary care.
The Care-at-Home Team
- Look for staff who are comfortable with technology, used to managing risk, and aim to solve problems.
This one is especially important for high acuity programs. The task of delivering acute care in patients’ homes often brings challenges that must be solved by the field nurse. To navigate this, these nurses should be comfortable making decisions and determining creative solutions to hurdles like few electrical outlets available to set up remote monitoring technology.
Listen to our clients at UMass Memorial discuss how their team built clinical confidence with treating acutely ill patients at home.
Patient Safety and Clinical Confidence in Hospital at Home
- Hold regular meetings to keep everyone synced.
Care at home programs often include a high degree of autonomy and coordination. Regular and frequent touch points are important for keeping the care-at-home team aligned on each patient’s care plan and the priorities of the day.
Staff report that daily huddles and weekly meetings are key to program success. These touch points help keep teams aligned and help to collaboratively address challenges. Include representatives from other teams that may support the care at home program, such as MIH paramedics, community service, or home care.
Care-at-Home Technology
- Drive adherence with accessible, patient-friendly technology.
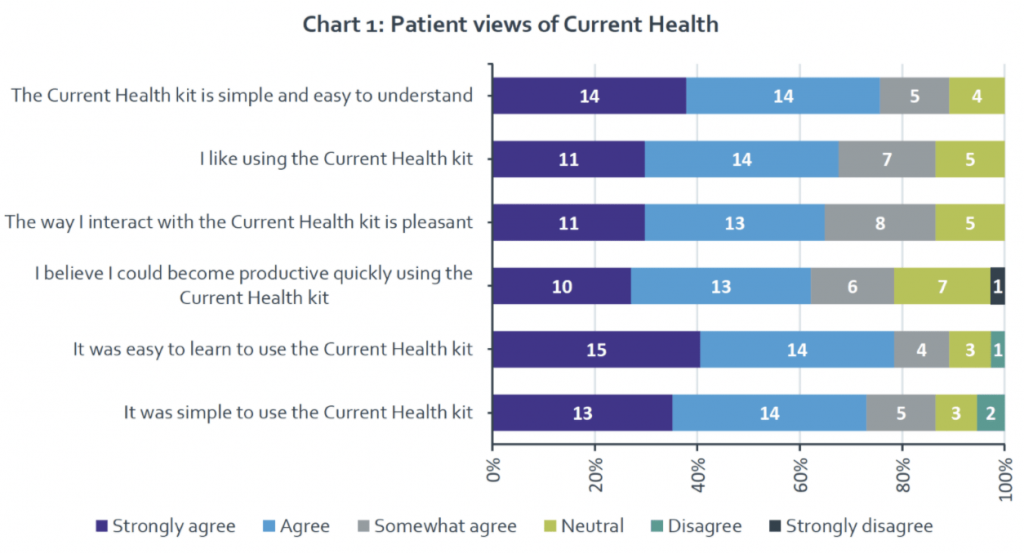
The technology that powers your care-at-home program has a significant impact on the patient and provider experience. To pursue equity and accessibility in your program, look for a technology partner that is easy to set up and understand, is configurable for various clinical pathways, and supports all aspects of the care at home experience.
- Train staff on monitoring and alarming.
Your care-at-home team must be comfortable with and confident in the technology you’re handing to patients. Allow for sufficient time to get staff acquainted with technology, including letting them experience the patient side of applications and monitoring devices.



![[Webinar Recording]This Way Home: Top 10 Predictions for Care at Home in 2025](https://www.currenthealth.com/wp-content/uploads/2025/01/DSG-846-JAN-WEBINAR-LINKEDIN-16_9-AD2-P2.jpg)